The US teen suicide rate is on the rise
Canva
The US teen suicide rate is on the rise
A sad teenage boy listening to music.
Over the past five years, suicide has been the second-leading cause of death for people ages 15-19 in the United States—second only to accidents. It might seem convenient or tempting to blame youth suicides on one headlining perpetrator—social media, the COVID-19 pandemic, bullying, or substance abuse, for instance—but the reality is much more complicated. It involves location, race, and socioeconomic status, among other compounding factors.
Certain groups are more at-risk than their peers. A survey from the Trevor Project in 2022 found that 45% of all LGBTQIA+ youth seriously considered suicide within the past year. Suicides amongst Black youth have also increased, partly due to increased racial discrimination and trauma radiating from incidents of public police brutality against Trayvon Martin, George Floyd, Breonna Taylor, Michael Brown, and many others.
Researchers are at work identifying the unique challenges teenagers face that put them at increased risk for suicide, as well as developing age-individualized solutions. In conjunction with the Biden administration’s Unity Agenda, the Health Resources and Services Administration recently updated its national guidelines to mandate suicide risk screening for those ages 12 to 21.
The Substance Abuse and Mental Health Services Administration pledged $7.3 million to a suicide prevention program focused on tribal youth and early intervention to aid students in juvenile justice systems, foster care, and mental health treatment centers.
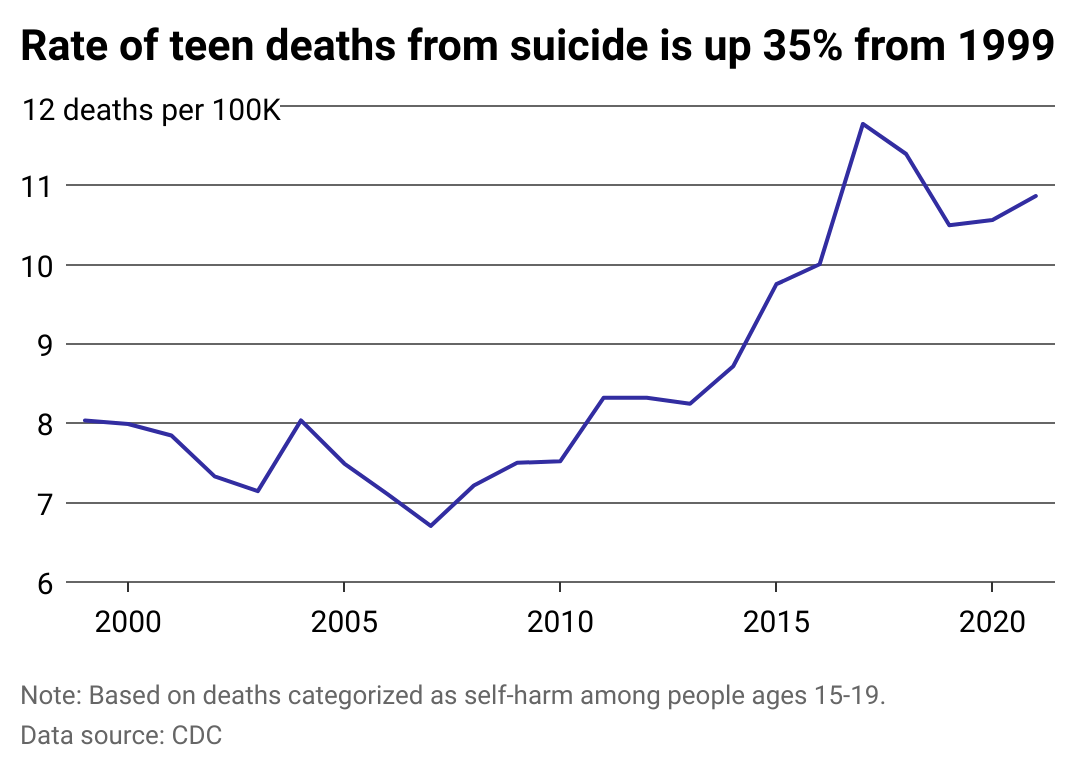
While the rate of deaths from suicides among teens is lower than the rate for the U.S. general population—14-15 deaths per 100,000 people in recent years, compared to 10-12 deaths per 100,000 15-19-year-olds—teen suicide has nonetheless traced an alarming upward trend since well before the onset of the COVID-19 pandemic—only to be further exacerbated thereafter.
Charlie Health examined the rising rate of suicide among adolescents, specifically looking at data for 15-19-year-olds citing data from the Centers for Disease Control and Prevention.
![]()
Charlie Health
The increase in teen suicide is the result of many factors
Line chart showing the rate of deaths from suicide among 15-19 year olds has grown 35%.
Social dynamics aside, teenagers have always been particularly vulnerable to suicide risk due in part to the physical developmental stage they are in. Teens have an underdeveloped prefrontal cortex—an area of the brain that does not fully develop until a person’s mid-20s—which can lead to increased impulsivity.
Combined with some significant stressors over the past two decades, it is possible to hypothesize reasons for the increase in youth suicide rates. However, it is unwise to pin the blame on any of these factors definitively.
Teenage suicides began to rise in 2008, coinciding with the economic recession. Teens experiencing a loss of perceived safety and general anxiety about the future—often due to feelings of instability—may have lead to an escalation in the number of youth suicides. Subsequently, the isolation and lack of socialization resulting from the pandemic, notably in its first year, conflated with factors such as climate change, increased frequency of school shootings, and rising student debt, are also thought to have contributed.
Youth suicide rates in Georgia, Indiana, New Jersey, Oklahoma, and Virginia were all higher during the pandemic than before.
Charlie Health
How states compare
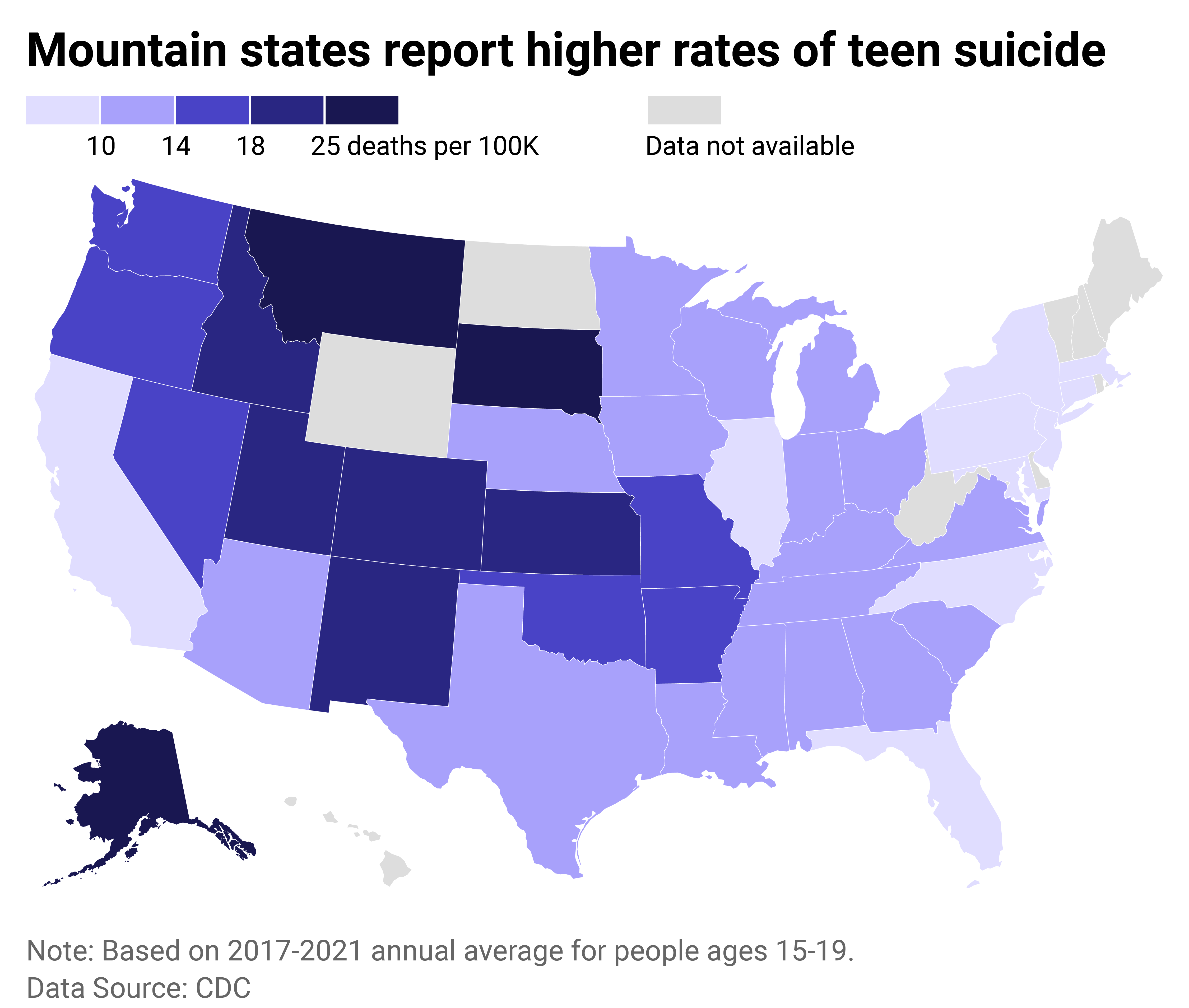
U.S. map of suicide rate among people ages 15-19. Alaska, Montana and South Dakota report highest rates.
The five highest-ranking states for teenage suicide, according to the latest CDC data, are Colorado (21.2 deaths per 100,000 youths), New Mexico (21.9), Montana (30.3), South Dakota (33.6), and finally Alaska, topping all 50 states with 39.8 deaths per 100,000 youths. One underlying cause of the relatively high rate of suicide in the mountain states is the region’s concentration of rural and often isolated communities.
From 2015 to 2019, urban suburbs and big cities had the lowest youth suicide rates. The community types with the most youth suicides tended to be more geographically scattered, relatively isolated groups, such as Native Americans, members of the Church of Jesus Christ of Latter Day Saints, strongholds of evangelical Christian practice, and farmlands in the Great Plains.
In these groups, teenagers may face more pressure to conform to traditional religious and gender roles. This fact, coupled with difficulty finding others to socialize with and increased access to firearms or living in a place where gun culture is deeply entrenched, boosts the risk levels for taking one’s own life.
Recognizing these unique factors, Montana Gov. Greg Gianforte recently allocated $2.1 million to the Rural Behavioral Health Institute to fund expanded capacity for mental health screenings and same-day urgent care in all schools across the state.
The Alaska Youth Suicide Prevention Program trains high school students to provide peer-to-peer suicide prevention in their classrooms, using the evidence-based Question Persuade Refer (QPR) method.
Charlie Health
Native teens face many unique challenges that are disadvantageous to their mental well-being
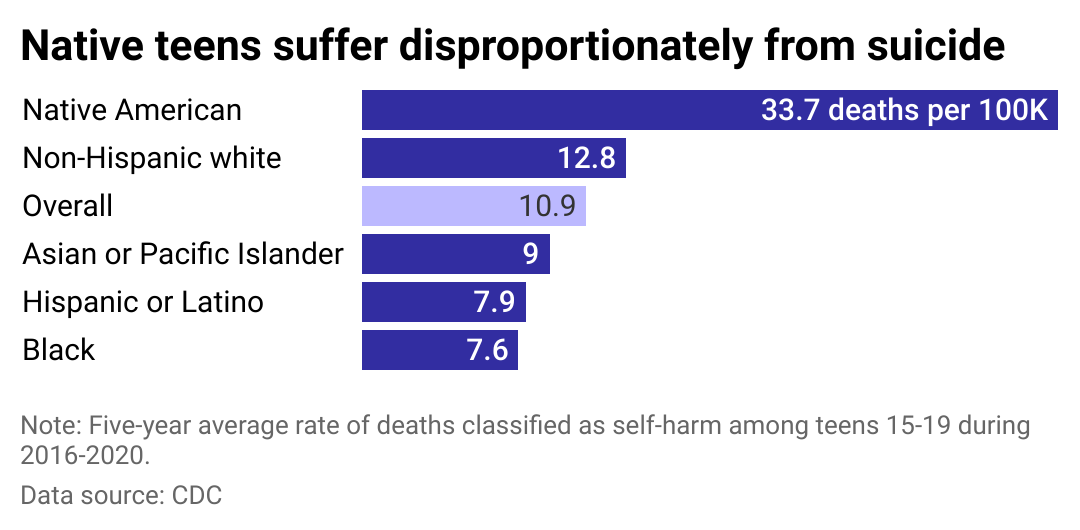
Bar chart showing the rate of deaths from suicide among Native teens is 3 times greater than the overall 15-19 year old population.
Suicide rates amongst Native American youth are alarmingly high, comprising the second-most common cause of death for Native youth ages 10 to 24.
Native teenagers face unique challenges that put them at higher risk for suicide than their peers, including intergenerational marginalization, resulting in increased rates of abuse, violence, and depression within their communities.
As a result, efforts to address high suicide rates amongst Native youth are also tailored specifically to their circumstances. The Center for Native American Youth encourages “community-based recognition programs,” including fellowships, competitions, and civic engagement training, to elevate local youth to feel empowered.
Grantees with the National Institute of Mental Health have outlined a framework for Native youth suicide prevention by strengthening community ties, including “a sense of belonging to one’s culture, a strong tribal/spiritual bond,” and “the opportunity to discuss problems with family or friends.”
This story originally appeared on Charlie Health and was produced and
distributed in partnership with Stacker Studio.