T-cell immunotherapy tied to 10-year remission in two leukemia patients, study finds
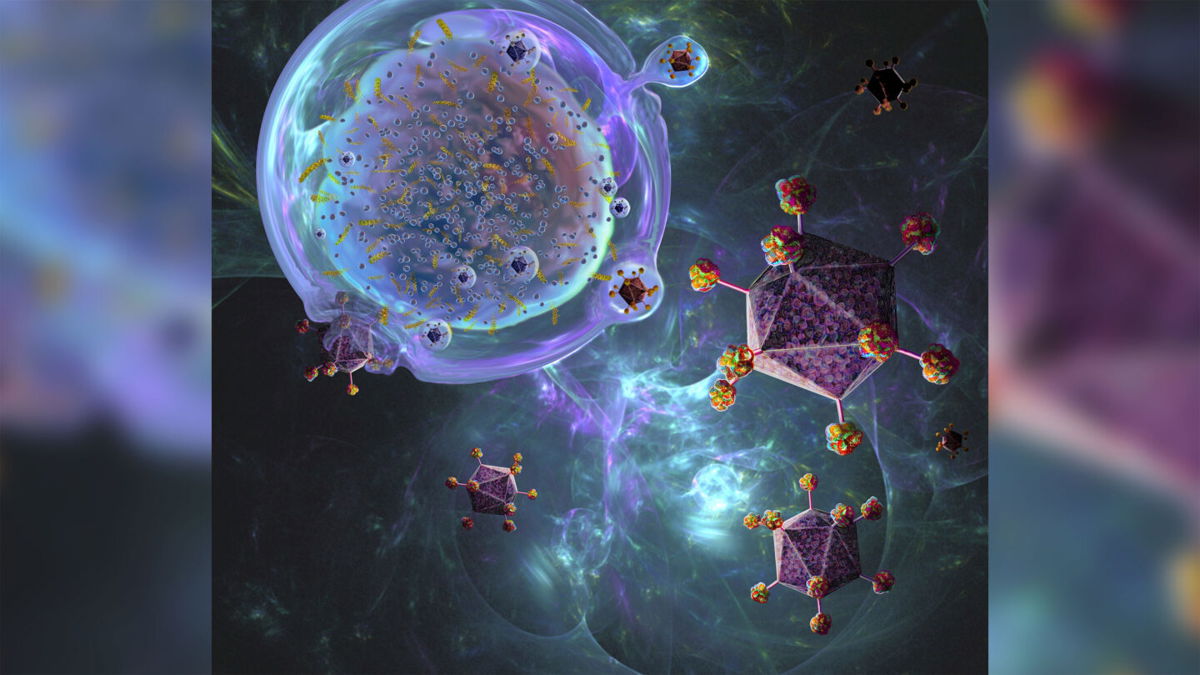
CAR-T cell therapy is a process being developed to treat cancer.
By Jacqueline Howard and Carma Hassan, CNN
Two people with leukemia achieved remission over a decade after being infused with CAR-T cells, immune cells that had been modified in a lab, according to a new study. The findings suggest that this approach could be a long-term therapy for leukemia — and some researchers describe it as a possible cure.
Chimeric antigen receptor or CAR-T cell therapy may be a “curative regimen” for chronic lymphocytic leukemia, according to the researchers, who announced their findings in a news briefing this week. Chronic lymphocytic leukemia accounts for about a quarter of new cases of leukemia.
The new paper describes “a 10-year follow up of the first patients we treated with CAR-T cells, chimeric antigen receptor modified T cells,” which is the “first cell therapy made from the patient’s own immune system,” Dr. Carl June, a cancer immunologist at the University of Pennsylvania and one of the study’s authors, said at the briefing.
Based on the study results, “we can now conclude that CAR-T cells can actually cure patients with leukemia,” June said.
The CAR-T cells are an immunotherapy treatment designed to treat leukemia by harnessing the body’s own immune system to target the cancer. The therapy sends a patient’s immune cells to a lab to be genetically modified using a virus and gives the cells the ability to recognize and kill the source of the cancer.
‘Sustained remission’
The new study, published Wednesday in the journal Nature, describes two distinct phases that the patients went through. They had an initial phase represented by CD8+ or CD4−CD8 CAR-T cells expressing a marker called Helios and then a shift into a long-term phase of remission dominated by the CD4+ CAR-T cell population.
“CAR T cells remained detectable more than ten years after infusion, with sustained remission in both patients,” the researchers wrote.
The researchers — from the University of Pennsylvania and the Novartis Institute for Biomedical Research in Cambridge, Mass. — studied the long-lasting T cells in the two people with leukemia who were in complete remission in 2010 after they had been infused with the cells as part of a Phase 1 clinical trial. The two remain in remission more than 10 years after the infusion, the researchers noted.
Oncologist Dr. David Porter, an author of the study, said this type of immunotherapy can come with serious side effects, though he said these therapies have become safer over the years and are given to hundreds or thousands of people a year.
One side effect is tumor lysis syndrome, “a phenomenon where you kill large numbers of cancer cells all at the same time and they spill their contents into the blood, and that can make people quite sick,” he said. Tumor lysis syndrome can cause electrolyte abnormalities and damage to the kidneys.
Another side effect is cytokine release syndrome, which gives people a severe flu-like syndrome, with very high fevers, nausea, vomiting, and muscle and joint pain.
“It can evolve to very dangerously low blood pressure, trouble breathing with fluid leaking into the lungs,” Porter said.
The third major side effect is a neurologic toxicity, leading to difficulty speaking or thinking clearly. In some situations, people can become comatose or develop seizures, according to Porter, but the majority of cases resolve on their own.
A ‘deeper understanding’
For the new research, June recruited Dr. Joseph Melenhorst to establish a laboratory that studied people who had been treated with CAR-T cells.
“We have actually built a pipeline and deeper understanding of the biology of the cells that were infused,” Melenhorst, of the University of Pennsylvania, who was an author of the new paper, said in Tuesday’s briefing. “We were able to isolate and analyze cells with new technologies, and it’s given a very good insight into some of the mechanisms of persistence and tumor response in both subjects.”
Doug Olson was one of the patients studied over the course of a decade. He was diagnosed with chronic lymphocytic leukemia when he was 49.
“Even though it was terrifying to hear that I had cancer, I really didn’t need a lot of treatment for about six years,” Olson said at the briefing.
Then “chemo got me in remission for another five years, and then things started to go downhill pretty quickly after that, and by 2010, about 50% of my bone marrow was CLL,” Olson said, referring to chronic lymphocytic leukemia, a type of cancer that starts from white blood cells in the bone marrow.
Olson said he was given his first infusion of CAR-T cells in September 2010 and shortly after was very sick and hospitalized for about three days — and the next week, his oncologist told him that no cancer cells were detected in his body.
“We did not think that this would be a curative therapy at all back in 2010,” June said.
“But the reason now I think we can say this is a cure for Doug — from a scientific point of view — is, I mean, these are the most mature, the oldest results available reported in the scientific literature, since they were the first treated,” he said. “So at this point, 10 years on, we can’t find any leukemia cells, and again, we still have the CAR-T cells that are on patrol and on surveillance for residual leukemia.”
The-CNN-Wire
™ & © 2022 Cable News Network, Inc., a WarnerMedia Company. All rights reserved.