What to do if your child is exposed to Covid-19 at school
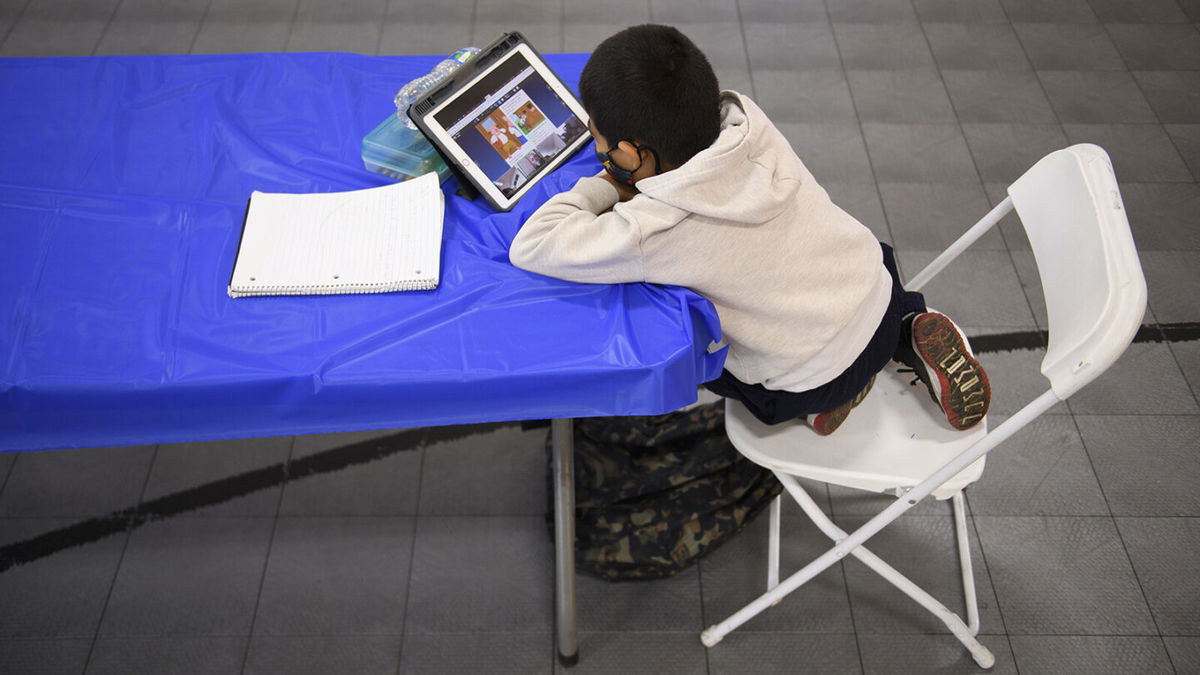
A child attends an online class at a learning hub inside the Crenshaw Family YMCA in Los Angeles
By Sandee LaMotte, CNN
Ping! It’s the email you’ve been dreading — your child may have been exposed to Covid-19 at school. How are you to cope with the possibility of 10 days of quarantine and the fear that your child — or another member of the family — may fall ill?
By being prepared, experts say. Here’s what you need to know and do.
Get ready now
Plan well in advance by setting up a structure in which all potential caregivers, including extended family members and friends, know their roles and expectations.
Provide every potential caregiver with a list of emergency phone numbers, including all family members, your health care provider, the local public health department, local hospital and ambulance service — just in case.
A fully vaccinated family member should be the primary caregiver for your child, said CNN Medical Analyst Dr. Leana Wen. Be sure to assign a backup in case the first choice is sidelined by work or other commitments.
If anyone in the family age 12 or older isn’t yet vaccinated, do so now, said Wen, who is an emergency physician and visiting professor of health policy and management at the George Washington University Milken Institute School of Public Health.
“Vaccination rate among kids 12 and older is really low,” she said. “Vaccinating that age group is an excellent way to protect younger children and vulnerable adults.”
It’s especially important for single parents to set up a network of fully vaccinated extended family, friends and neighbors who can help, Wen added.
“That way if you end up quarantined with your child, other people can help you with groceries and medications,” Wen said. “If you have friends who are single parents, consider offering to be their backup help. We are all in this together and need to help one another get through this time.”
Choose a room and stock up
Have a designated bedroom ready, preferably with a private bathroom that no one else will use. Stock the bedroom with all relevant forms of entertainment: TV, computer, iPad, books, even games that you could play via FaceTime or Skype.
Here’s a list of basic supplies to have on hand:
- A working thermometer to monitor fever, which is considered to be 100 degrees Fahrenheit (37.7 degrees Celsius)
- Fever-reducing medications, such as acetaminophen
- A box of rubber or latex disposable gloves and face masks
- Regular soap and at least 60% ethanol- or 70% isopropanol-based hand sanitizer (Antibacterial soap isn’t necessary if you wash properly, and that way you won’t contribute to the world’s growing problem of antibiotic-resistant superbugs.)
- Tissues to cover sneezes and coughs (But there is really no need to hoard toilet paper — this is a respiratory disease.)
- Regular cleaning supplies, kitchen cleaning gloves and trash can liners
- Disinfectant cleaning supplies: You can choose from a list that meets the virus-fighting standards of the US Environmental Protection Agency, or you can also make your own version by using 1/3 cup unexpired bleach per gallon of water or 4 teaspoons bleach per quart of water. Never mix bleach with ammonia or any other household cleaner — it produces toxic gases.
Picking up your child
The US Centers for Disease Control and Prevention recommended picking up your child from school alone, with car windows open for ventilation. If you do have other children with you, everyone should be masked unless they are under the age of 2.
If possible, stay in the car and have your child brought to you.
Once home, “wait 24 hours before cleaning and disinfecting your car, as that allows more time for the amount of virus in the air of your car to die off,” the CDC said.
Masks
For a time, anyone vaccinated did not have to worry about wearing a mask or getting tested after exposure to Covid-19. But that’s changed, Wen said.
“Now the CDC is saying that if you are vaccinated and exposed to somebody with Covid — which by definition if you’re taking care of a young child you’re certainly exposed — you need to get tested three days after the exposure. And in the meantime you should be wearing a mask in all public places.”
Why the change?
“Now we know that vaccinated people who are symptomatic from Covid-19 carry just as much virus as unvaccinated symptomatic people,” she said. “It true that the risk of getting Covid-19 is much reduced if you are vaccinated, but if you are exposed to an infected person and therefore could be infected yourself, you shouldn’t be interacting with others.”
Quarantine for vaccinated children
When should you quarantine? That’s complicated, Wen said, because it depends on whether the child is vaccinated.
“Let’s say that this is a 12-year-old who is fully vaccinated who had close contact with someone who tested positive for Covid-19,” Wen said. “According to the CDC, unless the child develop symptoms, he or she does not need to quarantine.
“So technically, by CDC guidelines, a child who is fully vaccinated with no symptoms can continue to attend school as long as he or she wears a mask at all times,” Wen said. “I understand that certain schools may have stricter protocols than that, and people should certainly follow their school guidelines.”
The vaccinated child should, however, be tested three to five days after the exposure, Wen said. But don’t test any earlier than that, she warned, because the virus would not have had time to incubate and the test would be inaccurate.
What type of test should you use? Rapid tests can give results within hours; PCR (polymerase chain reaction) tests typically take a day or so to get the results, because the respiratory sample is being examined for minute traces of virus. That makes PCR tests the current gold standard for Covid-19 testing.
“This is my opinion, but I would get a formal PCR test, not a rapid test, because the accuracy of the rapid test is generally less than the PCR test,” Wen said. “If what’s initially available to you is a rapid test, do that first. But it’s also a good idea to follow it up with a confirmatory PCR test.”
Quarantine for unvaccinated children
If an unvaccinated child is exposed to someone with Covid-19, the rules change, according to the CDC.
“The child should quarantine for 10 days, the amount of time the CDC recommends,” Wen said. “You can shorten the quarantine period to seven days, if the child has had a negative test that’s done at least five days after the exposure.”
Take, for example, a child who is exposed to a person with Covid-19 on Monday.
“If exposure was Monday, you can test the child on Saturday, and if it’s negative, the child can be back in school on the following Monday,” Wen said.
“But if you don’t get the child tested, then the quarantine period is 10 days. And during that period of time, you should not be in public if you are unvaccinated.”
If possible, keep the child away from other family members — hopefully in that separate bedroom and bathroom — and have the designated caregiver monitor for symptoms for the full 10 days.
Symptoms
Keep in mind that children may not have any noticeable symptoms at all. “As many as half of pediatric infections may be asymptomatic,” the CDC said.
When children do show symptoms, they are typically mild, but that doesn’t mean that a child cannot get seriously sick, the CDC noted.
Just like adults, children with preexisting conditions, such as “obesity, diabetes, asthma or chronic lung disease, sickle cell disease, or immunosuppression, might also be at increased risk for severe illness from COVID-19,” the agency warned.
Possible symptoms of Covid-19 infection are similar to many other viral infections and include fever, fatigue, headache, muscle or stomach pain, poor appetite, sore throat, cough, nasal congestion, shortness of breath, nausea, vomiting and diarrhea.
“Although children manifest many of the same symptoms of Covid-19 infection as adults, some differences are noteworthy,” the American Academy of Pediatrics said.
“According to the CDC, children may be less likely to have fever, may be less likely to present with fever as an initial symptom, and may have only gastrointestinal tract symptoms.”
One last, very important thing: Call 911 immediately if your child or another family member develops any of these symptoms:
- Increased or sudden difficulty breathing or shortness of breath
- A persistent pain or pressure in the chest
- Any sign of oxygen deprivation, such as new confusion, bluish lips or face, or you can’t arouse the sick person
Isolation
What happens if your child does develop symptoms or tests positive for Covid-19? Then the child needs to move from quarantine to full isolation, Wen said.
“Meaning your child should not be in school for 10 days after the onset of their symptoms or the positive test, even if they wear a mask,” she said. “And other children in the family should quarantine and not be going to school, if one child is known to be infected.”
An older child may be able to care for themselves, thus allowing caregivers to set food and drink outside the door, Wen said, adding that “if it’s a baby, toddler or younger child who needs a caregiver’s physical support, this will be harder.”
Vaccinated parents do not have to isolate, Wen said. However, they should follow the CDC guidelines to test three days after exposure and mask in public in the meantime.
In addition, caregivers should wear a face mask at all times when interacting with the child — even if they and other adults in the family are fully vaccinated, Wen said.
“When not able to keep away from others, a mask should be worn by all members of the household,” the CDC said.
Another good idea to reduce risk is to open as many windows and doors as possible to keep fresh air circulating, thus diluting any virus in the air.
“Being in a shared space with a child who is actively infectious, for long periods of time, exposes you to risk,” Wen said. “It may not be possible to limit time together or to physically distance, especially with a young child, so try to improve ventilation by opening windows and keep a mask on yourself.”
Although “direct contact and sharing air” are the main ways experts now believe Covid-19 is spread, Wen said, you can reduce risk for yourself and others in the household by following these tips from the CDC:
- Don’t share drinking glasses, cups, forks or other eating utensils.
- Don’t share towels or bedding.
- Don’t shake the isolated child’s dirty clothes to “minimize the possibility of dispersing virus through the air.”
- Wear disposable gloves when cleaning the child’s bedroom or bath, but then toss them before moving on to other cleaning chores. “Clean hands immediately after gloves are removed,” the CDC said.
- Dedicate a lined trash can for any tissues or other paper or disposable products used by an isolated or sick person, the CDC says, adding that caregivers should “use gloves when removing garbage bags, handling and disposing of trash. Wash hands after handling or disposing of trash.”
- Have everyone in the house wash their hands at every opportunity. Clean and disinfect all those commonly shared surfaces — don’t forget the refrigerator and microwave handles.
Keep everyone else in the home separate from the child and the adult caregiver who is caring for them for the period of the isolation, Wen said. Be especially cautious to protect people in the household who are unvaccinated or at high risk for severe outcomes from Covid-19.
“For example an immunocompromised child or older adult with severe underlying conditions — try to keep that person on the other side of the house or in some area where there is no shared public space,” Wen said.
When can your child go back to school?
That could depend on the extent of your child’s risk when exposed, subsequent symptoms, school policies and more, so keep in close contact with your child’s school and your pediatrician.
Minimum requirements by the CDC for a child with symptoms include the following:
- It has been at least 10 days since symptoms started
- Overall symptoms have improved
- The child has no fever for at least 24 hours (without fever-reducing medication)
The-CNN-Wire
™ & © 2021 Cable News Network, Inc., a WarnerMedia Company. All rights reserved.
This story has been updated from April.